Breast Cancer Patient
Lorem ipsum dolor sit amet consectetur adipisicing elit. Esse error reiciendis doloribus natus nihil maiores, totam amet! Numquam debitis unde nam consectetur, et deleniti quod, illum tempore non sint molestiae!

Say hello to simple ideas designed to help you live your happiest, healthiest life. From practical health tips to delicious recipes and heartfelt patient journeys, every piece exists to help you thrive—your way.
Lorem ipsum dolor sit amet consectetur adipisicing elit. Esse error reiciendis doloribus natus nihil maiores, totam amet! Numquam debitis unde nam consectetur, et deleniti quod, illum tempore non sint molestiae!

Lorem ipsum dolor sit amet consectetur adipisicing elit. Esse error reiciendis doloribus natus nihil maiores, totam amet! Numquam debitis unde nam consectetur, et deleniti quod, illum tempore non sint molestiae!
Lorem ipsum dolor sit amet consectetur adipisicing elit. Esse error reiciendis doloribus natus nihil maiores, totam amet! Numquam debitis unde nam consectetur, et deleniti quod, illum tempore non sint molestiae!
Lorem ipsum dolor sit amet consectetur adipisicing elit. Esse error reiciendis doloribus natus nihil maiores, totam amet! Numquam debitis unde nam consectetur, et deleniti quod, illum tempore non sint molestiae!
Lorem ipsum dolor sit amet consectetur adipisicing elit. Esse error reiciendis doloribus natus nihil maiores, totam amet! Numquam debitis unde nam consectetur, et deleniti quod, illum tempore non sint molestiae!
Lorem ipsum dolor sit amet consectetur adipisicing elit. Esse error reiciendis doloribus natus nihil maiores, totam amet! Numquam debitis unde nam consectetur, et deleniti quod, illum tempore non sint molestiae!
Lorem ipsum dolor sit amet consectetur adipisicing elit. Esse error reiciendis doloribus natus nihil maiores, totam amet! Numquam debitis unde nam consectetur, et deleniti quod, illum tempore non sint molestiae!
Lorem ipsum dolor sit amet consectetur adipisicing elit. Esse error reiciendis doloribus natus nihil maiores, totam amet! Numquam debitis unde nam consectetur, et deleniti quod, illum tempore non sint molestiae!
Lorem ipsum dolor sit amet consectetur adipisicing elit. Esse error reiciendis doloribus natus nihil maiores, totam amet! Numquam debitis unde nam consectetur, et deleniti quod, illum tempore non sint molestiae!

Hydrate before you feel thirsty. Try to drink at least a half-ounce of water for each pound you weigh. If you weigh 150 pounds, you should aim to drink a minimum of 75 ounces of fluids per day.
Monika Smith, DO, Emergency Medicine Physician
Discover expert insights, inspiring stories, health tips, and more by exploring the content below!









Are emotional ups and downs disrupting daily life? Learn common signs of mood disorders, and when to talk to a doctor about diagnosis and treatment options.




























When 20-year-old Krystal learned she needed a kidney transplant, her family turned to social media for help. Within days, Janet—a longtime friend of Krystal’s mother—stepped forward. She was a perfect match. Thanks to Virtua and the power of living donation, Krystal is embracing a second chance.
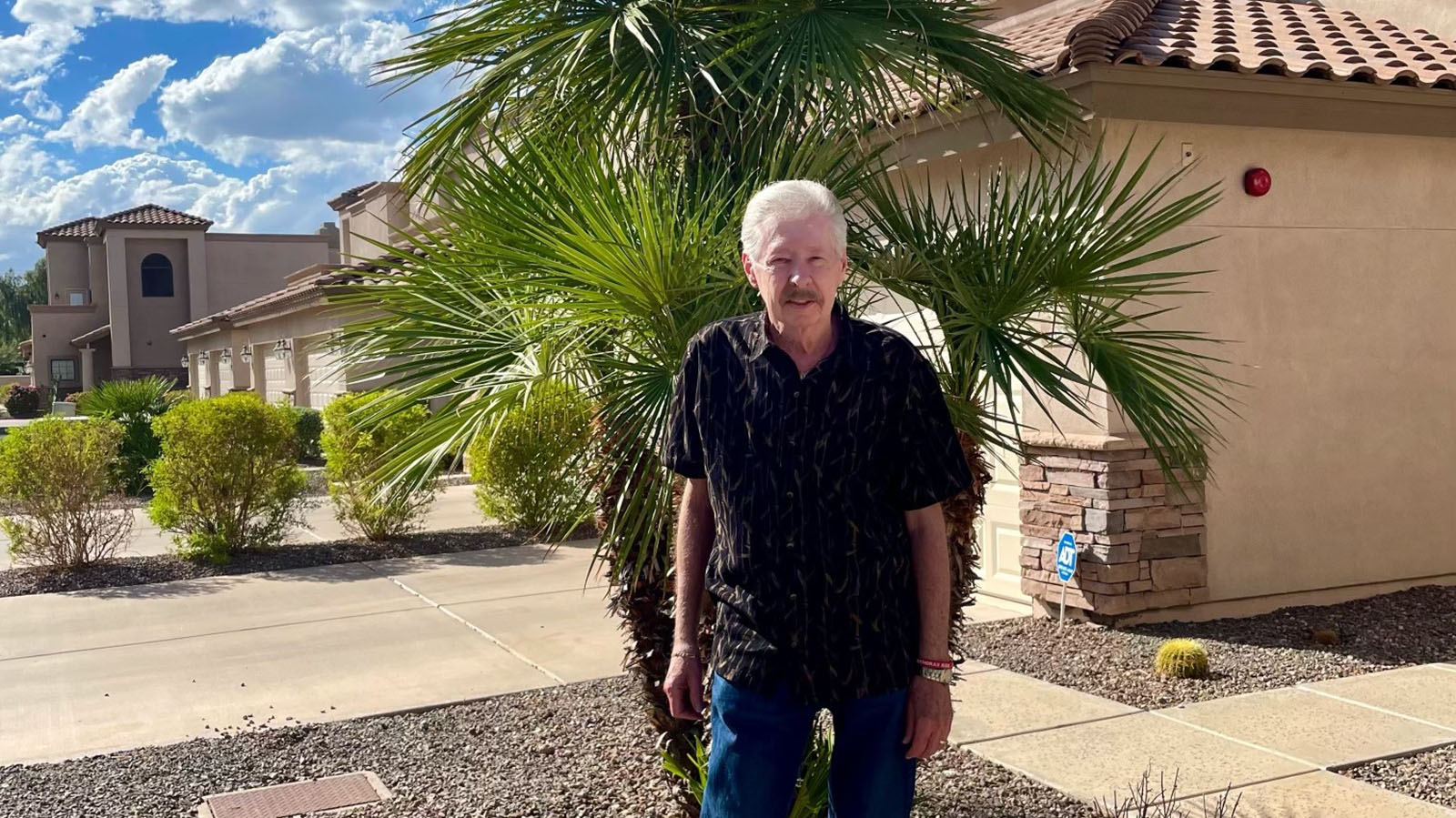
Frank was living with stage 4 COPD and just 17% lung function. Everyday moments like walking to the mailbox or playing with his granddaughter felt impossible. But after meeting Dr. Riaz, everything changed. Thanks to a minimally invasive valve procedure available at Virtua, Frank is breathing easier and embracing the moments that matter.
When Shannon moved to South Jersey, she was in search of a doctor who could help manage her ongoing health challenges, like ovarian cysts to fibroids. Finding a new doctor felt overwhelming—until she met Dr. Green at Virtua. They talked through all Shannon’s options and decided on a minimally invasive approach that made all the difference. Now, she’s back to living her life and reminding other women to put their health first.
Chris experienced high blood pressure well before his 40s, and unfortunately, it only worsened over time. Despite countless visits to doctors, he never found a solution. That was until he met Dr. Sanghvi. With a groundbreaking procedure, Chris received the care he needed. And just one week later, he felt better than ever—more active, more relaxed, and more productive at work.
For Tina, hearing the word "cancer" was terrifying, but Dr. Gleimer offered relief. With a personalized approach and clear expertise, Dr. Gleimer eased Tina’s fears and mapped out a plan. After a successful radical hysterectomy and no need for chemotherapy or radiation, Tina is thriving. She calls Dr. Gleimer her "buddy for life."
Join our Good Vibes community today to receive personalized, medically-reviewed content delivered straight to your inbox.
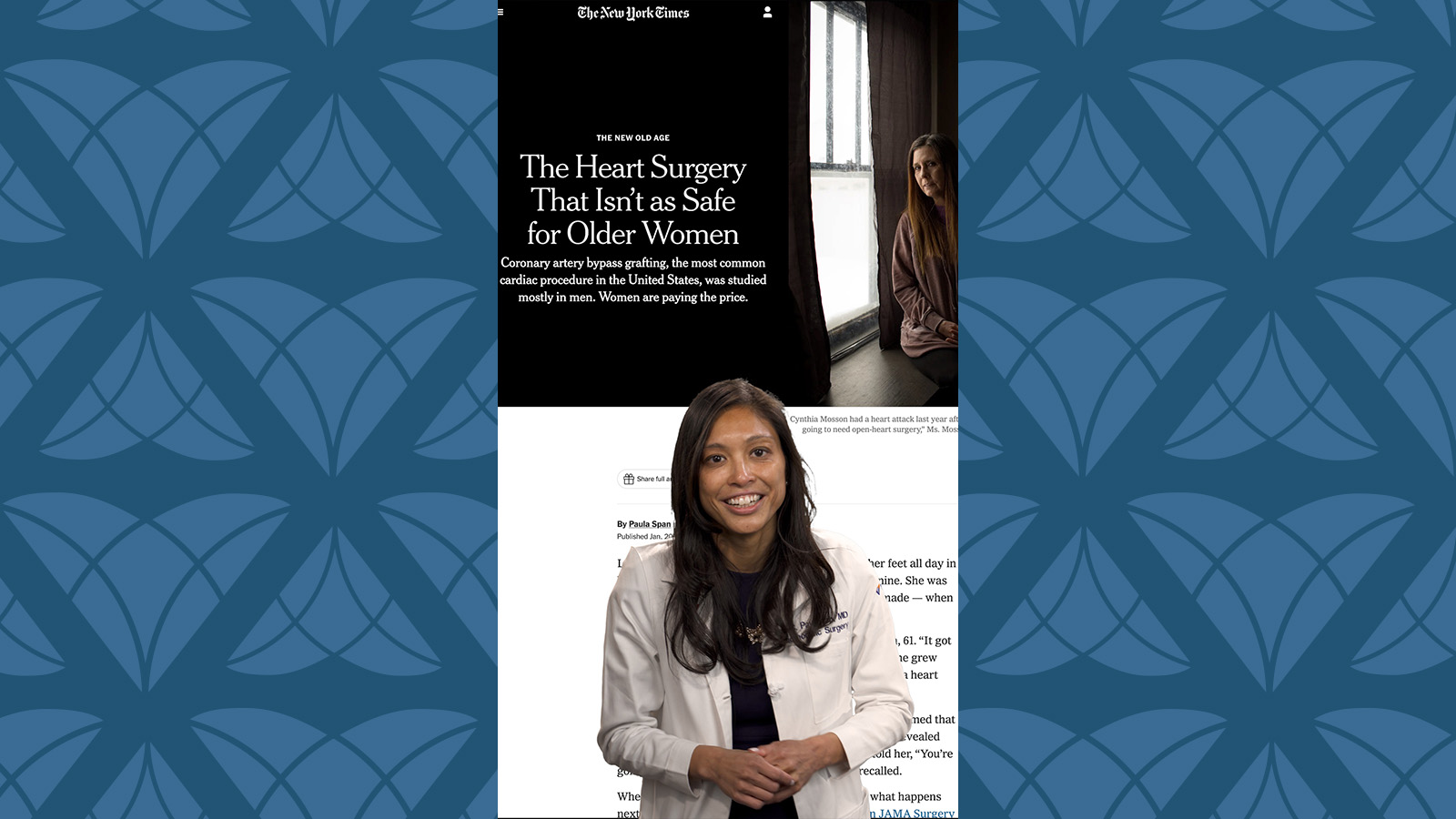
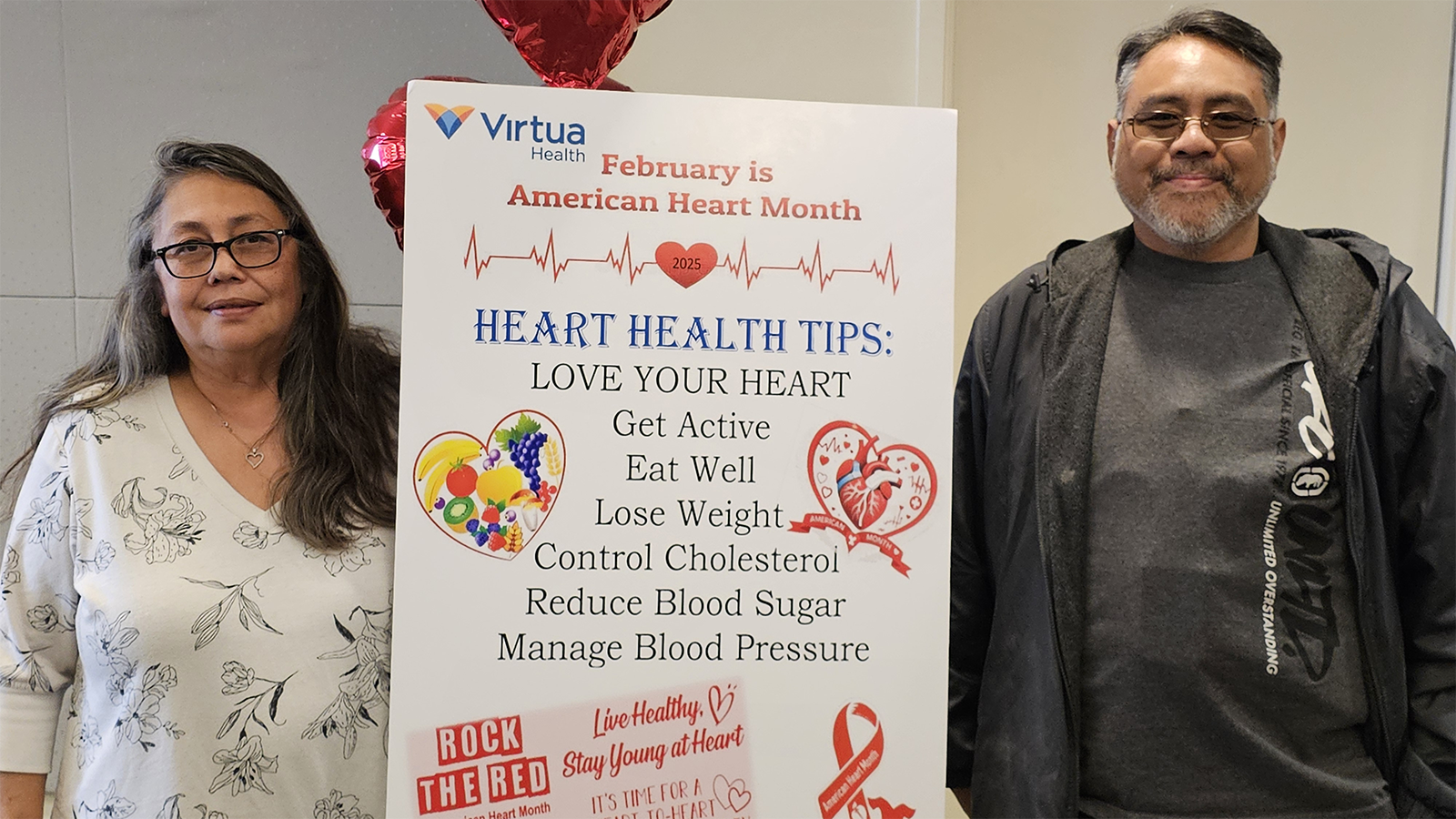
HeartTalk magazine helps you stay well through a focus on living a healthy lifestyle, with the latest expert advice on preventing and managing heart disease and much more.
There's always something happening at Virtua Health! Explore support groups, health seminars, educational sessions, live events, and more.
