Get Pumped! Assist Devices Can Improve Heart Failure Symptoms
Heart failure can leave you weak and unable to take part in the activities you enjoy. Left ventricular assist devices, or LVADs can improve symptoms and keep you out of the hospital.
Theresa Rowe, MSN, CRNP, Director, Heart Failure Program
If you have heart failure, your heart is weakened and unable to pump enough blood to meet your body’s needs. As a result, even the easiest activity can leave you exhausted.
Nowadays, a small mechanical pump, called a left ventricular assist device (LVAD), is providing a boost to people living with heart failure.
An LVAD takes over the workload of the left ventricle, pumping blood to the vital organs, just like the normal heart would. Previously, these devices were very big and noisy, with many moving parts.
Because of their size and complexity, there was a greater likelihood that mechanical issues would arise. For that reason, these devices started out as a “bridge” for people waiting for a heart transplant.
Today, with the advent of smaller mechanical pumps with only one moving part that last for years, the pumps can be used as “destination” therapy, working alongside other treatments to improve people’s lives.
Small Size, Big Power
The LVAD is the size of a D battery. It is implanted inside your chest and is attached to the left ventricle and the aorta (the main artery that carries oxygenated blood from the heart to the rest of the body). A thin cable connects the pump to a controller, which regulates pump flow, speed, and power. The LVAD is powered by long-lasting batteries or connection to an electrical outlet.
The pump’s motor turns 5,000 to 10,000 revolutions per minute, depending on the type of LVAD that is implanted. Because the LVAD provides a continuous flow of blood, it may be difficult to feel a pulse. Blood pressure is measured using a Doppler ultrasound.
The continuous blood flow allows people with an LVAD to breathe more easily, feel less fatigued, and have improved exercise tolerance. Many are able to return to work or resume most normal activities.
Specialized, Shared Care
LVADs are designed for patients who have end-stage (refractory) heart failure. These individuals no longer respond to traditional medical therapy and require more support than what medications can provide.
Patients with refractory heart failure may be eligible for a transplant. However, the relative cut-off for a heart transplant is 65, and many people we treat are 75 and older. They also may not want a transplant, or cannot undergo two significant heart surgeries. The LVAD can be their solution.
Ordinarily, patients are required to travel to the hospital where they received their LVAD for follow-up visits, as well as minor and elective procedures. Many are nervous about traffic, parking, and logistics surrounding these appointments.
Through our “shared care” program, we care for people implanted with LVADs at other hospitals. Our clinicians are specially trained on the mechanics of the device, how certain medications and procedures can affect its operation, and how to best maintain their overall health. These patients also can undergo less-invasive and same-day procedures here at their local hospital.
Heart failure treatment has greatly evolved. Through medications, attention to diet, exercise, and implantable devices like special internal defibrillators and the LVAD, we are better able to manage heart failure, reduce heart failure admissions to the hospital, and improve quality and quantity of life.
Your Heart, Our Focus
Our team of heart failure experts focus on improving your quality of life and reducing your risk of being admitted to the hospital. Learn more here about our heart failure program or call 888-847-8823 to make an appointment.
There's So Much More to Explore
Discover expert insights, inspiring stories, health tips, and more by exploring the content below!

Can Your Gut Health Affect Your Heart?
A complex interplay between the bacteria that live in our intestines and the systems in our body can influence our risk for serious illnesses, including cardiovascular disease. Here's how to stay on track.

How the Unique Stages of a Woman's Heart Affect Her Health
Heart disease is gender-blind, affecting women and men at equal rates. But the reasons why women get heart disease may be different from men.

Complex Aortic Surgery Provides Lu’Shell Hope for the Future
A life-threatening tear in Lu’Shell’s aorta was discovered during twice-a-year cardiac tests. Complex open-heart surgery at Virtua ensured she'll have more time to focus on her family.

HeartTalk Magazine
HeartTalk magazine helps you stay well through a focus on living a healthy lifestyle, with the latest expert advice on preventing and managing heart disease and much more.

Are You Eating Too Much Salt? High-Sodium Foods to Watch For
Salt hides in many everyday foods. Some high salt foods are obvious, others are meal staples you may not expect. See what foods you should avoid.

4 Exercise Tips to Help You Reverse High Blood Pressure
A high blood pressure diagnosis often comes with daily prescription medications. However, for some, improvements in diet and exercise alone may be enough to reverse that.

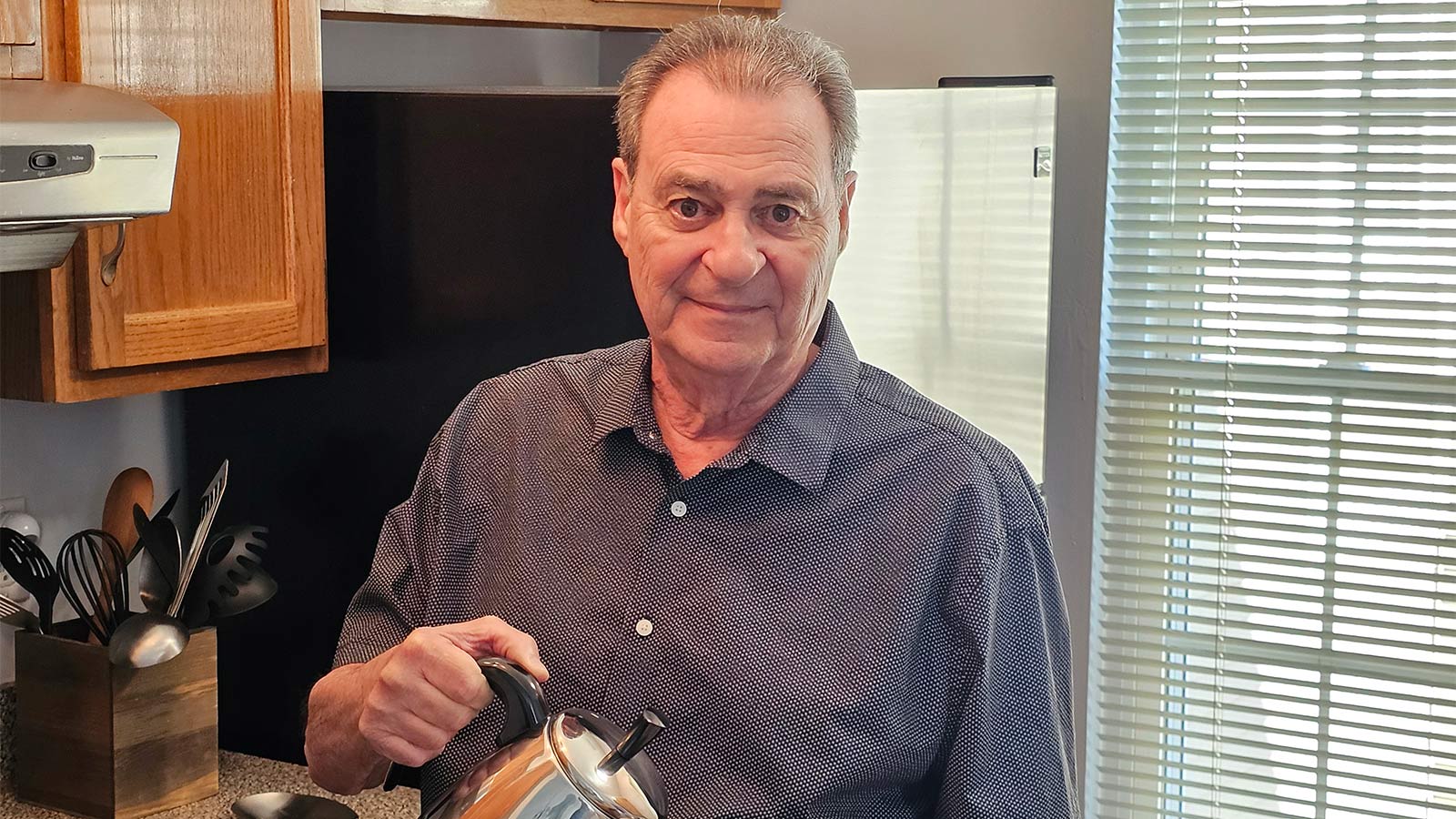
Timely Heart Care During a Heart Attack Helps Joe Feed the Community
Joe Gilbert runs his Burlington Township store with a schmear of goodness. He didn't let a heart attack and coronary artery bypass surgery stop him from donating Brooklyn-style bagels to local organizations and food banks.

3 Reasons Why Now's the Time to Find Relief From Varicose Veins
If you have varicose veins, the season to wear shorts and swimsuits can bring pain and embarrassment. Here are some tips to provide relief, and when you might want to undergo a medical procedure so your legs can be ready for next summer.

Lifesaving Heart Care Creates a 'Bond That's Never Left Us'
Cancer treatment created scarring that damaged Stanley Ollek's heart and blood vessels. The Virtua cardiac team never gave up on restoring his health.

How High Blood Pressure Affects Your Body
High blood pressure, also known as the "silent killer," often goes unnoticed as many patients mistakenly believe that a lack of symptoms means they’re in the clear. This dangerous misconception can result in severe health consequences if left unmanaged.

5 Interesting Facts About Your Heart
Think you know everything about your heart? Here are five surprising facts that might change the way you care for your ticker.

Get to the Bottom of Blood Pressure Numbers
Which blood pressure number is more important? Both systolic and diastolic pressures can indicate risk for heart disease. Virtua Cardiologist Troy Randle, DO, explains more.
CABG Surgery: What Women Should Know About Heart Health and Healing
An informative guide on CABG surgery with a focus on the unique challenges and experiences women face before, during, and after the procedure.

When to Take Action for a Stronger Heart
Subtle symptoms like jaw pain, indigestion, and shortness of breath can be signals of serious heart problems. Dr. Rita Butler, an interventional cardiologist, at Virtua Cardiology, explains the key red flags that should never be ignored when it comes to your heart health.

Groundbreaking Renal Denervation Procedure Controls a Lifetime of High Blood Pressure
Toning down overactive sympathetic nerves that run along the kidney arteries reduced Chris Grosso's blood pressure to normal levels.
Patient Story: LVAD Mechanical Pump Strengthens Michael's Heart Function
A left ventricular assist device bolstered Michael Hinchliffe's blood flow, improving his stamina and quality of life.

Mitral Valve Surgery Keeps Yaneth Living the American Dream
An active mom and restaurant owner, Yaneth Ramos placed her loved ones' well-being before her own. When a doctor detected a heart murmur, Virtua cardiologists ensured she received the best treatment for her mitral valve prolapse so she could safely return to her busy life.
Inside Look at Blood Vessels Aids PAD Treatment
A new treatment for peripheral vascular disease that gives doctors a real-time, inside view of your blood vessels has given Daniel Spillane a leg up on enjoying life.
Denise Davis: Pay Attention to Your Heart Health
Denise Davis didn’t think she was at risk for heart disease. But after a heart attack and bypass surgery, she urges others to pay attention to their heart health.

Sweet Music: Trust, Teamwork Save Justin from Heart Attack
Justin Fisher rarely gave his health much thought. But when tests revealed he had potentially life-threatening clots in three arteries, he was glad he had a team of caring doctors in his corner.
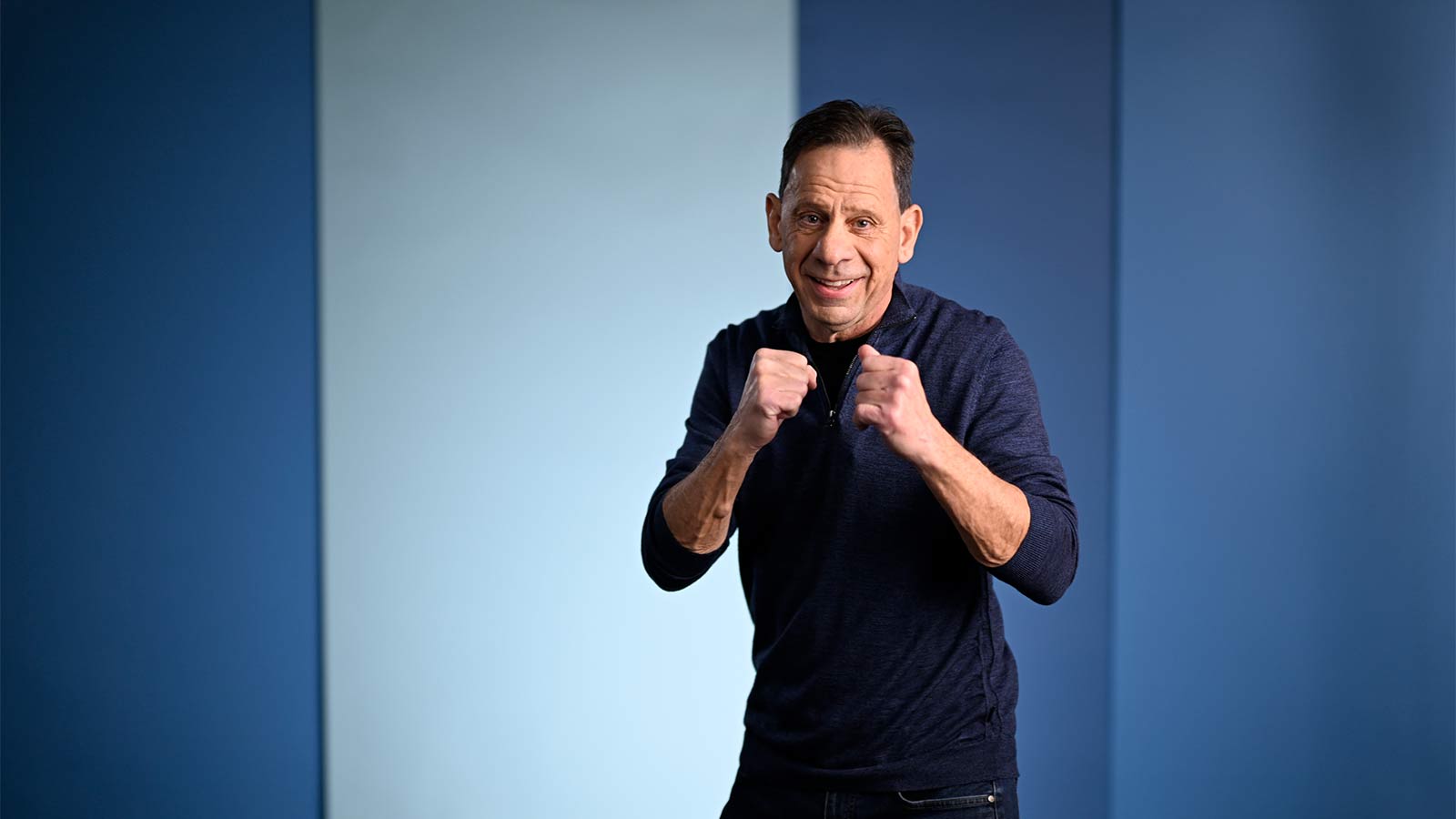
Complex Heart Surgery Nets James a Lifelong Friend
Jimmy Palma is a full-contact athlete, but a tear in his aorta nearly benched him for good. Thanks to heart surgery at Virtua Our Lady of Lourdes, he’s back in the game.

8 Key Steps to Better Blood Pressure Control
Chronic high blood pressure greatly increases your risk for heart attack or stroke. Virtua cardiologist Rozy Dunham, MD, advises how to keep your blood pressure under control.

Signs You Should Get Treated For Vein Problems
Painful, bulging veins in your legs are not just a cosmetic concern. They could be a sign of a more serious condition that requires treatment. Here’s what you need to know.

One New Heart Valve Saves Two Lives in the Tritten Family
A South Jersey woman needed a new heart valve while pregnant. Experts from Virtua Health performed the first-of-its-kind procedure—saving the lives of both mother and baby.

What You Need to Know About Heart Failure
Heart failure can have some easy-to-miss symptoms, so when should you take note and see a doctor? Tolulope Agunbiade, MD, FACC, explores some common questions and answers.

6 Numbers Key to Keeping Your Heart Healthy
What if there were a handful of numbers that could help you track your heart health? See how these tests and actions can strengthen your heart and prevent problems down the road.

Five Mindfulness Tips That Can Help Heal Your Heart
It’s OK to feel upset at times. But if your emotions are too frequent or intense, your heart could pay the price. Virtua cardiologist Hafeza Shaikh, DO, offers some tips to heal both the mind and the heart.

Watchman Heart Device: a Technological Breakthrough for Blood Clot Prevention
Atrial fibrillation, or AFib, is a heart rhythm disorder that can increase chances of a stroke. Cardiologist Heath Saltzman, MD, discusses the Watchman device, an innovative medical implant for AFib that can save lives.
Albert's Emergency Cardiac Surgery Is a 'Story of a Lifetime'
Timely rescue and emergency aortic dissection surgery at Virtua Our Lady of Lourdes Hospital saved Albert’s life.

Love Your Heart: Essential Care Tips for Every Stage of Life
Heart-healthy habits boost your well-being now, and set you up for better health later in life. And they’re as good for your children and aging parents as they are for you.

How Do I Measure My Blood Pressure at Home?
Checking your blood pressure at home is key to managing hypertension. Virtua cardiologist Vasu Palli, DO, has good advice on finding a good monitor and how to measure your blood pressure correctly.

How Do I Improve My Cholesterol Levels?
When it comes to your cholesterol, there's the good (HDL) and the bad (LDL). Learn how boosting your good cholesterol number can help lower your bad cholesterol number.

3 Ways to Reduce Your Stroke Risk
Working with your doctor, you can live a healthier lifestyle and explore medical options to reduce your risk for stroke.
Advanced Heart Failure Therapies Get Bernadine Back to Full Speed
Thanks to guideline-directed medical therapy, including an implanted device to regulate and synchronize her heartbeat, Bernadine heart function has returned to normal.

Keeping the Beat: Advanced Heart Surgery for Aortic Aneurysm
A problem with your aortic root can disrupt the flow of blood throughout your body, leading to shortness of breath, chest pain, and more. Virtua cardiothoracic surgeons are among the few specialists in the region performing valve-sparing aortic root replacement.

Heart-Healthy Summer Recipe: Hummus and Veggies
This creamy hummus is not just heart-healthy – it’s downright delicious! Pair it with your favorite veggies for a nutritious boost.

4 Delicious Heart-Healthy Recipes Perfect for Summer
Searching for easy to make, heart-healthy recipes for your next summer party or BBQ? Discover these creative and guilt-free summer dishes that are perfect for keeping your heart healthy while enjoying tasty seasonal flavors!

Heart Healthy Summer Recipe: Dessert Parfait
If you’re in search of a healthier sweet treat to enjoy this summer, look no further than this heart-healthy parfait. It’s rich and decadent yet surprisingly light, making it the perfect indulgence for warm days!

Heart-Healthy Summer Recipe: Pear and Walnut Salad
Packed with antioxidants and fiber, this heart-healthy salad is as satisfying as it is guilt-free! Light, refreshing, and low in sodium, it’s the perfect summer meal to enjoy any time.

Heart-Healthy Summer Recipe: Terrific Turkey Burgers
Switching to turkey is an easy, low-sodium alternative to beef that tastes just as great. Give this twist on a turkey burger a try for your next gathering!
Atrial Fibrillation and Stroke: What's the Connection?
Atrial fibrillation increases your risk of stroke. Virtua cardiologist Darius Sholevar, MD, explains why, and how nonsurgical treatments to restore your heart’s rhythm.
Heart Tests Your Doctor May Order
Just like a mechanic checking your car, your doctor performs tests to assess your heart health. Virtua cardiologist Samuel Ventrella, MD, explains the most common tests your doctor may order.
Managing Pregnancy for Mothers With Heart Conditions
Discover how today's advances in maternal-fetal medicine make it possible for women with heart conditions to have healthy pregnancies.

Heart Healthy Recipe: Basil Pesto Pasta With Seared Vegetables
Homemade pesto is a great option when it comes to making heart-healthy food choices. Try this pasta recipe for a delicious and healthy meal.

Heart Healthy Recipe Chocolate Avocado Chia Pudding
Satisfy your sweet tooth without sacrificing flavor with this pudding that includes avocado and chia seeds, giving this decadent dessert a sneaky, heart-healthy boost.
Keep Your Heart Rhythm in Check With Your Smartwatch
Smartwatches started out as a great way to track your exercise. Now, they can help monitor your heart health. Virtua cardiologist Aatish Garg, MD, explains how.
Mind Your Meds for Blood Pressure Risks
If you have high blood pressure, it’s important to know what’s in over-the-counter medications and the effects they can have on your heart health.
Magic Pill for Heart Health? Cut 300 Calories a Day
A new study found that consuming just 300 fewer calories—the equivalent of six Oreo cookies or three Reese’s Peanut Butter Cups—each day can help protect your heart and curb your diabetes risk.
3 Smart Ways to Boost Your Heart Health
Your heart is the hardest working muscle in your body. With this wholehearted advice, you can keep it healthy and strong throughout your life.
3 Best Exercises For Heart Health
Whether you exercise to shed pounds, relieve stress, or live healthier, here are some of the best exercises you can do to help your heart health by improving blood flow and lowering blood pressure.

Get Your Heart Pumping With These 25 Workout Songs
One of the best ways to stay heart healthy is to add some aerobic exercises to your weekly routine. We put together this blood-pumping, heart-thumping, pulse-pounding playlist to help you get moving.
Your Chest Pain: Heartburn, Heart Attack, or Something Else?
The burning sensation in your chest after eating a big meal is probably a passing case of heartburn. But it could be something else that should be checked by a doctor.
3 Heart Healthy Recipes to Win Valentines Day
No matter how you're celebrating Valentine's Day, you can treat yourself to delicious, heart-healthy food with these recipes.
How Work and Home Stress Can Affect You
While we can’t always take away stress, how we deal with it matters. Learn how to tame your stress and positively impact your health.
Why Improving Your Health Is Going To The Dogs And Cats
Bonding with pets can have positive effects on your physical and mental well-being, including improving your cardiovascular health. Learn how your pet can get your heart pumping.
Why Younger Women Need Start NOW To Safeguard Their Hearts From Heart Attacks
New research shows that younger women in the U.S. are experiencing heart attacks at a higher rate than they were 20 years ago. See how you can take steps now to safeguard your heart.
Can You Die of a Broken Heart?
Cases of broken heart syndrome—sudden, intense chest pain triggered by an emotionally stressful event—are on the rise. Here’s what you should know.
Mitral Valve Surgery Opens Doors for Improved Quality of Life
Virtua cardiothoracic surgeons use advanced, minimally invasive procedures to treat mitral valve conditions, keeping you and your blood headed in the right direction.
6 Healthy Habits to Start in Your 20s for Better Lifelong Health
These expert tips will help you establish healthy habits in your 20s that can help you crush your health goals now and in the future. Get started today.
Do You Have a Fatty Heart?
There’s usually no hiding from fat. But a type of fat we can’t see can harm our heart health. Virtua cardiologist Thomas Galski, DO, has steps you can take to keep going strong.
Get Pumped! Assist Devices Can Improve Heart Failure Symptoms
Heart failure can leave you weak and unable to take part in the activities you enjoy. Left ventricular assist devices, or LVADs can improve symptoms and keep you out of the hospital.
A Cardiologists Advice on Heart-saving Emergency Cardiac Care
It's understandable why people are afraid to go to the ER during this pandemic. But, if you have the symptoms of a cardiac emergency, it's vital—and safe—to get immediate help.
Virtua Doctor’s Experience Is a Warning for All About COVID-19 and Strokes
Virtua cardiologist Troy Randle, DO, didn't think he would get COVID-19—but he did. He certainly didn't expect the life-threatening stroke that followed.
You May Feel Fine, but Gregory Says "Don't Skip Your Medical Care"
For a large family in Beverly, Burlington County, doctor visits were sometimes too expensive. But they learned the importance of regular medical care after a cancer diagnosis and cardiac issues.
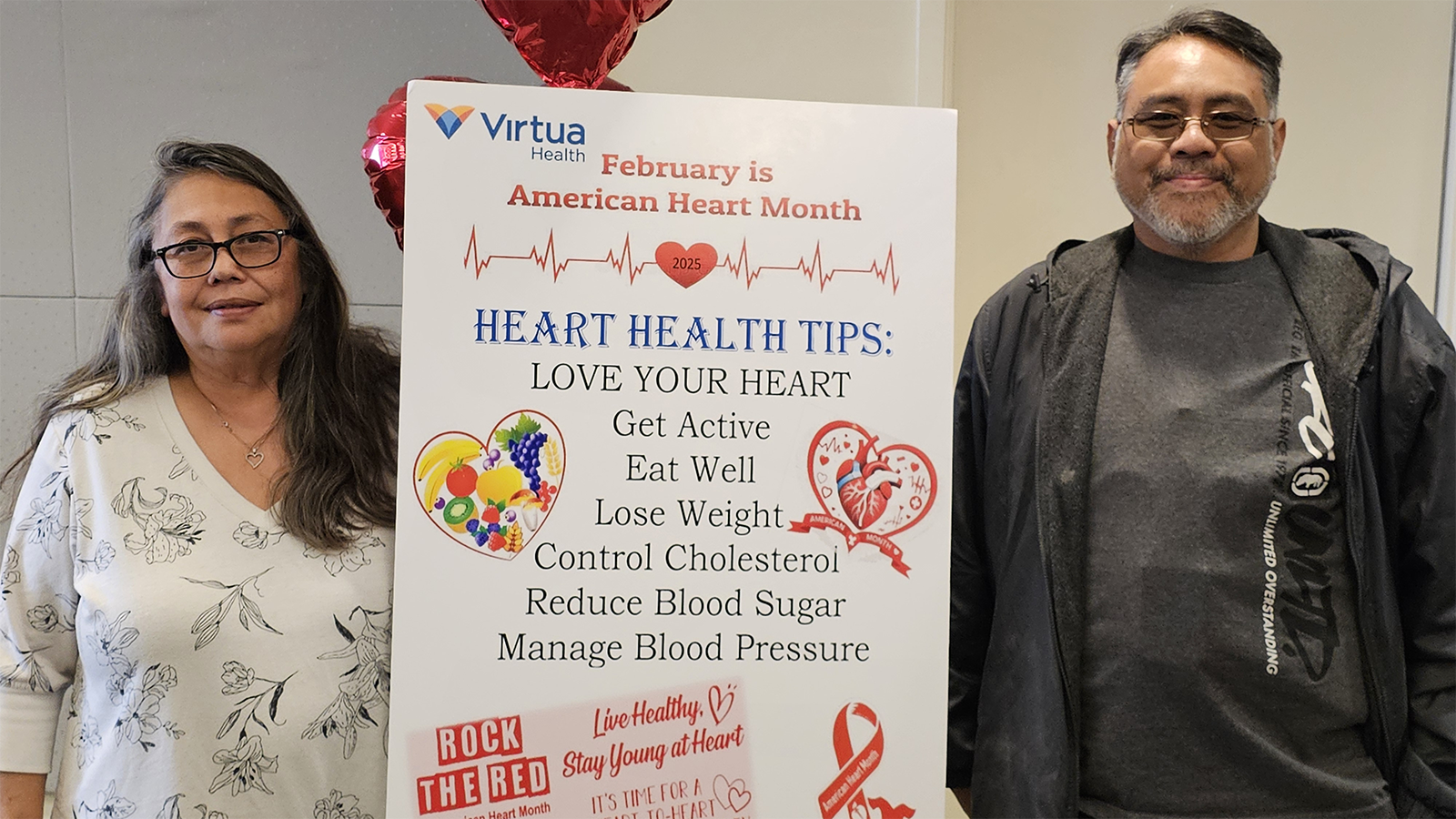
In Sickness and in Health: Couples Often Share Heart Disease Risk
Couples share a lot more than romance. They often have the same behaviors and risk factors that can lead to heart disease. Cardiologist Michael Horwitz, DO, offers three ways to team up for your health.
"Reduce Your Heart Disease Risk With a Plant-based Diet"
Plant-based diets rich in fresh fruits and vegetables, whole grains, and legumes can lower your risk for heart disease. Virtua cardiologist Rozy Dunham, MD, FACC, can help you make the switch.
Hybrid Robotic Heart Surgery and Valve Replacement Restores Quality of Life
A complex robotic-assisted coronary artery bypass and TAVR helped carpenter Edward Owens shape his future.
Can Marijuana Hurt Your Heart Health?
Cannabis is now legal in many states but that doesn't mean it's good for your health. Virtua cardiologist Donald Orth, MD, explains the risks and how it can affect your heart.
6 Tips for Restoring Your Heart Rhythm
AFib is the most common type of abnormal heart rhythm. Virtua cardiologist Dr. Delcine Sood explains how medication and lifestyle changes, and procedures if needed, can help you manage AFib.
Eat Smart for Your Heart
Knowing which foods to eat more of and which foods to limit is a powerful way to prevent heart disease and improve your overall health. Here are six easy ways to eat smart for your heart.
Cardiac Rehab: Strengthening Your Heart After Leaving the Hospital
If you've had a heart attack, cardiac rehab is an important part of the recovery process. Through medically supervised exercise, lifestyle education, and support, you can return to your daily activities.
Your Heart Needs A Good Nights Sleep
Struggling with sleep? Lack of sleep can raise your risk for heart attack, stroke, heart failure, depression, and other health issues. Virtua cardiologist David Lawrence, MD, offers tips to catch more Z's.
Are You at Risk for AAA—the Silent Killer?
The aorta is the largest blood vessel in your body. If an aneurysm, or weakness, in the aortic wall bursts, it can lead to a life-threatening emergency. Learn about the risks and available treatments at Virtua.
The Cardio Oncology Team Protects Your Heart During Cancer Treatment
Cardio-oncology combines the expertise of cardiologists and oncologists to help protect the hearts of people undergoing cancer treatment. Learn more.
Get Relief From Painful Varicose Veins This Summer
For people who have varicose veins, especially women, the season to wear shorts and swimsuits can bring pain and embarrassment. Get a leg up on pain relief with these tips.
Exercise Your Way to a Stronger Heart
Today, we know that exercise is safe for patients with heart failure and can help relieve symptoms. Robert Mohapatra, MD, Virtua Cardiologist, shares tips to be more active with heart failure.
Fish Oil: A Good Catch or a Scam?
Millions of Americans take fish oil supplements to help prevent heart disease. But do they really work? Talya Spivack, MD, Virtua Health cardiologist, offers some insight.
My Heart Seems to Skip a Beat - Should I Be Worried?
Most heart palpitations can be explained by external factors. But they can also be a sign of a potentially serious condition. Virtua Cardiologist Hafeza Shaikh, DO, offers more information.
Menu Planning? Try These 5 Heart-smart Substitutions
Food can be medicine and plays a big role in keeping our hearts healthy. Erin Wickersham, RD, Virtua Health registered dietitian, offers five ways you can start improving your heart health with food.

5 Health Risks Tied to Weight
While nearly four in 10 Americans are obese, it shouldn't be viewed as the new normal. It comes with a steep cost that you pay for with your health and life.

Heart-Healthy Recipe: Maple Orange Salmon With Mango Salsa
Salmon is packed with heart-healthy omega 3 fatty acids and tends to be more flavorful than other fish. Try this recipe for a delicious and healthy fish dish.
Do Not Wait to Get Help When a Stroke or Heart Attack Strikes
Fear of contracting COVID-19 should NOT stop you from seeking emergency medical care—especially if you're feeling the symptoms of a heart attack or stroke.
4 Reasons Why Heart Patients Should Follow COVID 19 Safety Guidelines
If you have heart disease, you should be extra vigilant in following COVID-19 prevention guidelines.
Young Mother Finds Support for Anxiety After Rare Cardiac Event
Susan Campbell experienced a rare, but life-threatening, cardiac issue that was treated successfully. While she regained full health, she worried it could happen again. See how she got support.
Is Your Heart Age Older Than You?
You can calculate your “heart age” by tallying up your risk factors for heart attack and stroke. That number shows the years of strain you've added to your heart.
Heart Healthy Recipe: Mediterranean Shrimp Salad
Eating smart doesn’t mean eating bland food. This tasty recipe is packed with bold flavor, and it’s low in fat.
