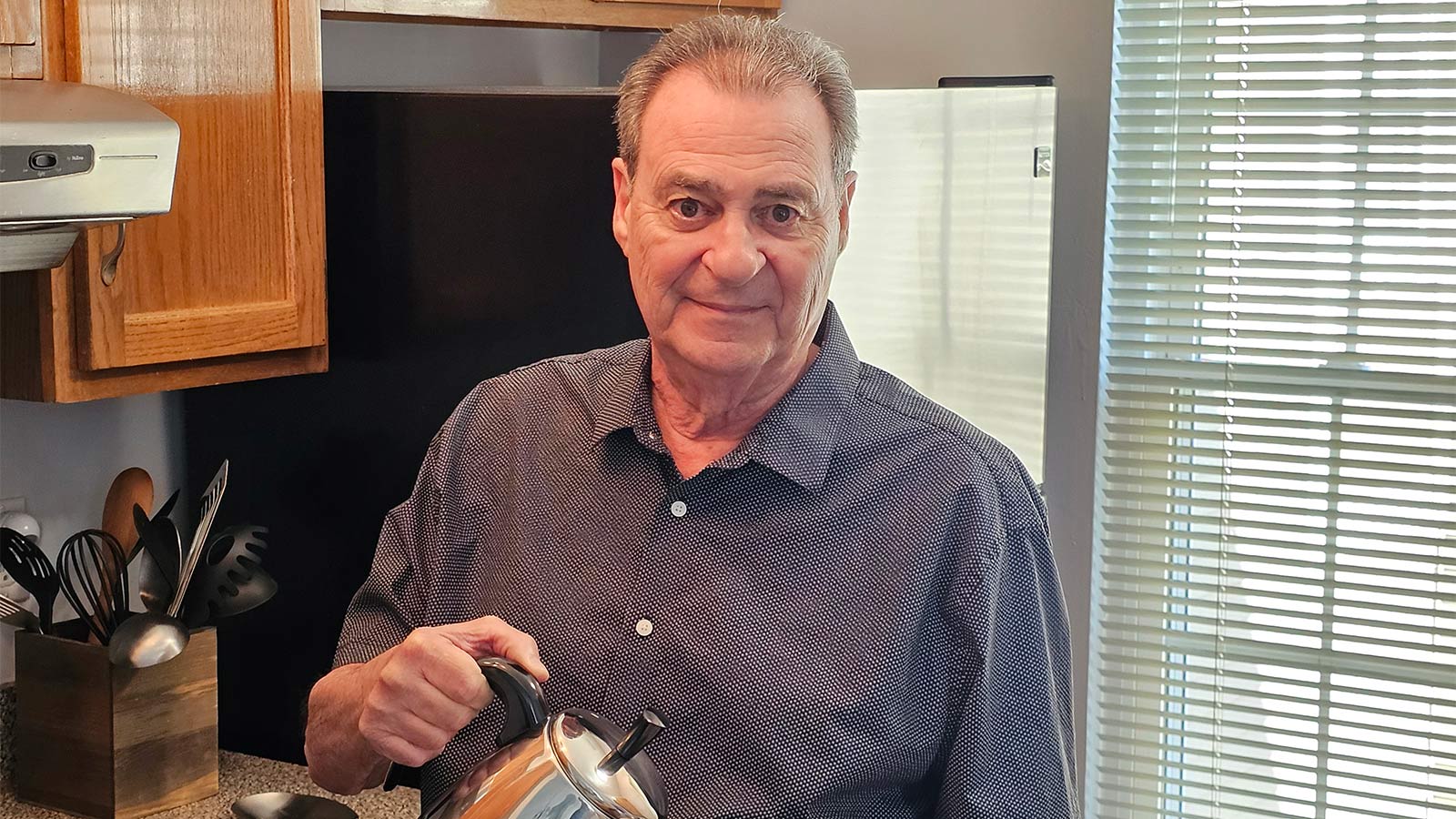
Hybrid Robotic Heart Surgery and Valve Replacement Restores Quality of Life
A complex robotic-assisted coronary artery bypass and TAVR helped carpenter Edward Owens shape his future.
A carpenter and Army veteran, Edward Owens said he “felt pretty good for being old. But I couldn’t get over being tired for doing nothing.”
Owens’ fatigue, it turned out, was caused by several conditions that prevented his heart from pumping enough oxygen-rich blood to the rest of his body. In August 2020, the cardiac team at Virtua Our Lady of Lourdes Hospital in Camden performed a unique hybrid surgery on the 73-year-old Cape May resident: a robotic-assisted coronary artery bypass and a transcatheter aortic valve replacement (TAVR).
“Mr. Owens was starting to deteriorate pretty rapidly from the calcified valve and the blockage in his artery,” said Arthur Martella, MD, chief of cardiothoracic surgery at Virtua’s Camden hospital. “The fact we were able to fix both problems at the same time allowed him to recover more quickly from a lot of the symptoms and issues he was having.”
The dual, 4½-hour procedure involved meticulous planning among specialties, including a dry run.
“Everything went smoothly because we had prepared. We had things ready: plans A, B, and C,” said Ibrahim Moussa, DO, FACC, FSCAI, RPVI, an interventional cardiologist and medical director of the Structural Heart Program at Virtua.
Now, six months later, Owens is once again in good health.
“I feel great. I have energy,” he said.
A History of Heart Problems
Owens learned as early as 2016 that calcium had built up around his aortic valve. His doctors from U.S. Department of Veterans Affairs (VA) informed him that if the valve prevented proper blood flow through his heart, he would need to have it replaced.
Dutifully, Owens received regular cardiac ultrasounds and electrocardiograms. Each test confirmed the diagnosis. In July 2019, while on an extended trip to Florida, Owens first began to experience unexplained fatigue.
“I thought I was just getting old,” he said. “But in May 2020, I went to the VA clinic in Cape May, and they told me to go to the hospital. I told my daughter, and she set everything up with Dr. Moussa at Virtua.”
Dr. Moussa ordered an echocardiogram and, in July, determined Owens had more than aortic valve disease. He also suffered from coronary artery disease, pulmonary hypertension, and poor right ventricular function (heart failure). His ejection fraction — the squeeze of his heart pumping out blood — was only 30 percent. A healthy ejection fraction is 50 to 75 percent.
“With aortic stenosis, the heart has to work harder to squeeze enough blood through a valve that isn’t opening well. If you have a blockage to the artery feeding the heart, there isn’t the supply of blood the heart needs,” said Dr. Martella. “The combination of aortic stenosis and coronary disease can lead to a rapid progression of symptoms.”
Imperative Intervention
Dr. Moussa recommended Owens go to the emergency room at Virtua Our Lady of Lourdes Hospital, where, on July 30, he had a pacemaker implanted to regulate his heart rate. Owens stayed in the hospital for a few days and returned home to recover.
The Virtua cardiac team then focused on treating Owens’ valve and coronary artery disease. Due to his age and condition, Owens was deemed too high risk for open-chest surgery. This type of surgery requires temporarily stopping the heart and using a heart-lung bypass machine.
“It’s like an old car that has been running for a long time. Sometimes when it stalls, it can be challenging to get it started again,” Dr. Moussa said of using the bypass machine. “We didn’t want to traumatize his heart.”
So the team planned a combined TAVR procedure and a coronary artery bypass using the da Vinci robotic surgical system. The da Vinci uses a high-definition 3D camera and a system that directly translates the surgeon’s hand, wrist, and finger movements to instruments inserted into the body through small incisions.
The Aug. 10 procedure occurred in the hospital’s advanced hybrid operating room. Dr. Moussa and Dr. Martella said Owens risked complications if they performed the surgeries separately.
The team decided to perform the TAVR first to lessen the time Owens spent under general anesthesia and relieve stress on the heart. Once Owens received the new valve, his pulmonary pressure decreased to a point where they felt it was safe to proceed with the robotic-assisted bypass.
Dr. Martella, who has performed more than 1,000 robotic-assisted cardiac surgeries, used the da Vinci Robotic System to harvest the left internal mammary artery and connect it beyond the blocked artery, restoring blood flow. The location of the blocked artery behind the heart made the surgery particularly challenging, noted Dr. Martella.
“With 90 to 95 percent of robotic surgeries, the artery is at the front of the heart,” he said. “This procedure would have been extremely difficult without the robot. With the robot, we are able to do surgeries like this much more efficiently, and less invasively.”
A Remarkable Recovery
Owens was discharged from the hospital four days after surgery, and within a month had a heart ejection fraction in the normal range.
“Procedures like this are a significant leap forward in being able to manage patients with multiple problems through less-invasive means,” said Dr. Martella.
Owens said he no longer feels tired and is back to performing small carpentry jobs.
“I’d recommend that hospital to everyone,” he said. “They are caring and loving. They were really fantastic.”
To learn more about Virtua Health’s comprehensive heart program, visit virtua.org/heart.
There's So Much More to Explore
Discover expert insights, inspiring stories, health tips, and more by exploring the content below!

How to Reduce Inflammation to Lower Your Risk of Heart Attack and Stroke

Specialized Pregnancy Care for Thaysnara’s Cardiomyopathy

Can Your Gut Health Affect Your Heart?

How to Use OTC Pain Relievers Safely: Acetaminophen vs. NSAIDs Explained

How the Unique Stages of a Woman's Heart Affect Her Health

Complex Aortic Surgery Provides Lu’Shell Hope for the Future

HeartTalk Magazine

Are You Eating Too Much Salt? High-Sodium Foods to Watch For

4 Exercise Tips to Help You Reverse High Blood Pressure

Timely Heart Care During a Heart Attack Helps Joe Feed the Community

3 Reasons Why Now's the Time to Find Relief From Varicose Veins

Lifesaving Heart Care Creates a 'Bond That's Never Left Us'

How High Blood Pressure Affects Your Body

5 Interesting Facts About Your Heart

Get to the Bottom of Blood Pressure Numbers
CABG Surgery: What Women Should Know About Heart Health and Healing

When to Take Action for a Stronger Heart

Groundbreaking Renal Denervation Procedure Controls a Lifetime of High Blood Pressure
Patient Story: LVAD Mechanical Pump Strengthens Michael's Heart Function

Mitral Valve Surgery Keeps Yaneth Living the American Dream
Inside Look at Blood Vessels Aids PAD Treatment
Denise Davis: Pay Attention to Your Heart Health

Sweet Music: Trust, Teamwork Save Justin from Heart Attack
Complex Heart Surgery Nets James a Lifelong Friend

8 Key Steps to Better Blood Pressure Control

Signs You Should Get Treated For Vein Problems

One New Heart Valve Saves Two Lives in the Tritten Family

What You Need to Know About Heart Failure

6 Numbers Key to Keeping Your Heart Healthy

Five Mindfulness Tips That Can Help Heal Your Heart

Watchman Heart Device: a Technological Breakthrough for Blood Clot Prevention
Albert's Emergency Cardiac Surgery Is a 'Story of a Lifetime'

Love Your Heart: Essential Care Tips for Every Stage of Life

How Do I Measure My Blood Pressure at Home?

How Do I Improve My Cholesterol Levels?

3 Ways to Reduce Your Stroke Risk
Advanced Heart Failure Therapies Get Bernadine Back to Full Speed

Keeping the Beat: Advanced Heart Surgery for Aortic Aneurysm

Heart-Healthy Summer Recipe: Hummus and Veggies

4 Delicious Heart-Healthy Recipes Perfect for Summer

Heart Healthy Summer Recipe: Dessert Parfait

Heart-Healthy Summer Recipe: Pear and Walnut Salad

Heart-Healthy Summer Recipe: Terrific Turkey Burgers
Atrial Fibrillation and Stroke: What's the Connection?
Heart Tests Your Doctor May Order
Managing Pregnancy for Mothers With Heart Conditions

Heart Healthy Recipe: Basil Pesto Pasta With Seared Vegetables

Heart Healthy Recipe Chocolate Avocado Chia Pudding
Keep Your Heart Rhythm in Check With Your Smartwatch
Mind Your Meds for Blood Pressure Risks
Magic Pill for Heart Health? Cut 300 Calories a Day
3 Smart Ways to Boost Your Heart Health
3 Best Exercises For Heart Health

Get Your Heart Pumping With These 25 Workout Songs
Your Chest Pain: Heartburn, Heart Attack, or Something Else?
3 Heart Healthy Recipes to Win Valentines Day
How Work and Home Stress Can Affect You
Why Improving Your Health Is Going To The Dogs And Cats
Why Younger Women Need Start NOW To Safeguard Their Hearts From Heart Attacks
Can You Die of a Broken Heart?
Mitral Valve Surgery Opens Doors for Improved Quality of Life
6 Healthy Habits to Start in Your 20s for Better Lifelong Health
Do You Have a Fatty Heart?
Get Pumped! Assist Devices Can Improve Heart Failure Symptoms
A Cardiologists Advice on Heart-saving Emergency Cardiac Care
Virtua Doctor’s Experience Is a Warning for All About COVID-19 and Strokes
You May Feel Fine, but Gregory Says "Don't Skip Your Medical Care"
In Sickness and in Health: Couples Often Share Heart Disease Risk
"Reduce Your Heart Disease Risk With a Plant-based Diet"
Hybrid Robotic Heart Surgery and Valve Replacement Restores Quality of Life
Can Marijuana Hurt Your Heart Health?
6 Tips for Restoring Your Heart Rhythm
Eat Smart for Your Heart
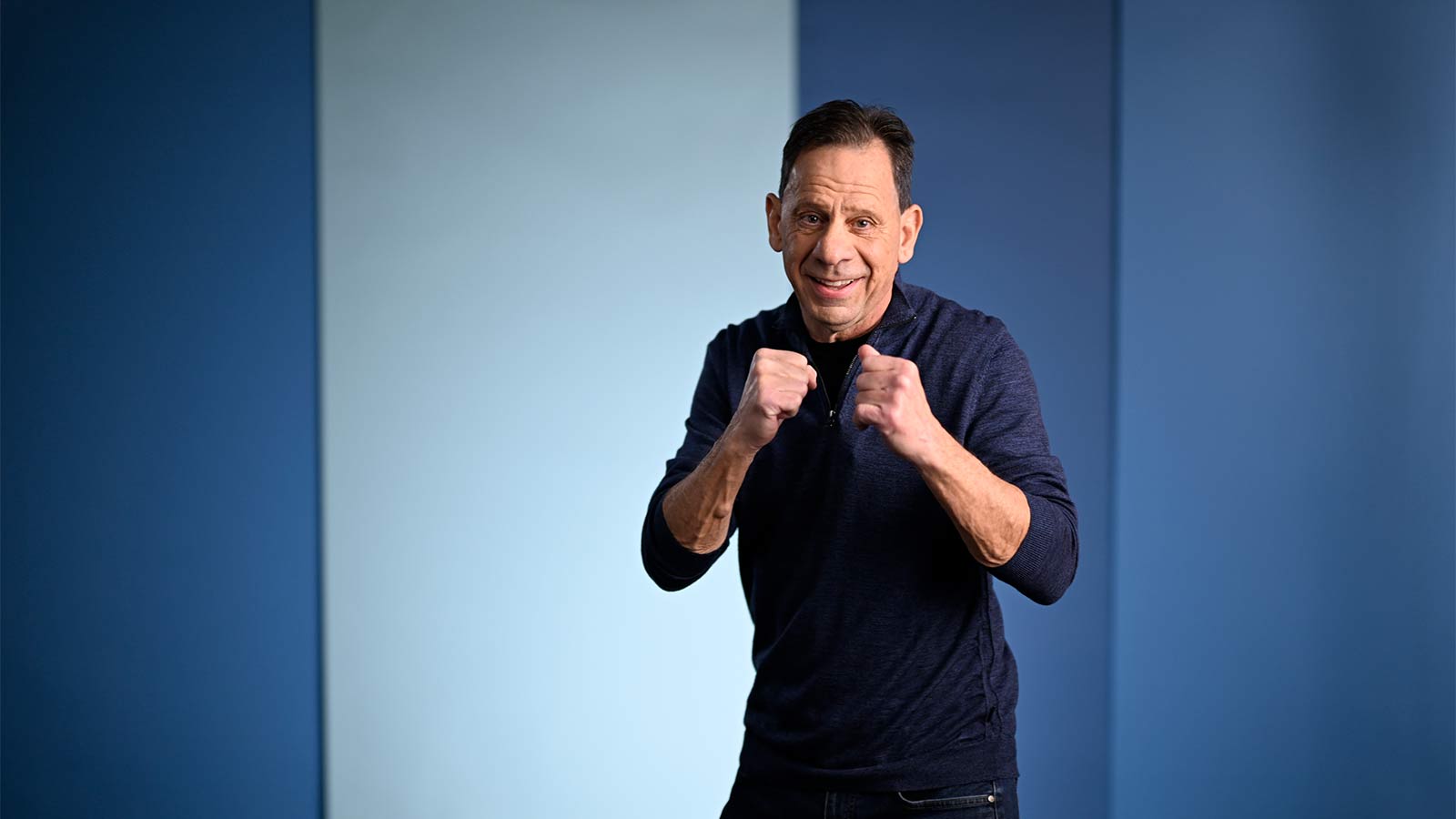
Cardiac Rehab: Strengthening Your Heart After Leaving the Hospital
Your Heart Needs A Good Nights Sleep
Are You at Risk for AAA—the Silent Killer?
The Cardio Oncology Team Protects Your Heart During Cancer Treatment
Get Relief From Painful Varicose Veins This Summer
Exercise Your Way to a Stronger Heart
Fish Oil: A Good Catch or a Scam?
My Heart Seems to Skip a Beat - Should I Be Worried?
Menu Planning? Try These 5 Heart-smart Substitutions

5 Health Risks Tied to Weight

